The value of private equity (PE) deals in the healthcare sector
has grown from 1 Barring government intervention, PE in healthcare
is here to stay.
It is no secret that PE firms’ primary focus is to create
transactional value. Additionally, the goals of private equity
differ from the more complex parameters faced by traditional health
providers in delivering care across a broad spectrum of payers and
patients.
Yet, health systems can learn from the ways private
equity firms introduce structural changes to the operational and
business model of acquired companies to reduce operating expenses,
compensate physicians, introduce technological enhancement, and
transition to value-based care.
Understanding these specifics may help legacy providers thwart
the shift of profitable services away from health systems and
enhance their operational models. Perhaps most importantly, it can
reestablish traditional providers as the go-to partnership
opportunity for primary care and specialty physicians.
1. Private equity focuses on parts of the market that are
fragmented, which gives room for pricing opportunism and creates
value through consolidation.
Providers are often fragmented geographically, which allows
private equity funds to consolidate market power and strive for
economies of scale. For example, ophthalmology has been a
particularly attractive specialty to PE investors because it is a
highly fragmented specialty: 68% of all eye care services are
performed by independent eye care providers who work mainly in
small practices.2
Typically, private equity firms seek to acquire a larger
physician practice to serve as their “platform” to drive
consolidation. The firm will then acquire smaller practices to gain
market share and expand brand recognition. This consolidation
strategy affords private equity the opportunity to negotiate
favorable contracts with insurers and medical suppliers, lower
overhead, increase utilization, and expand ancillary revenue
streams.
Private equity acquisition of physician practices was associated
with increased healthcare spending and utilization, according to a
study published in JAMA Health Forum. The study found a 20.2%
increase in charges per claim, an 11% growth in the allowed amount
per claim, and a 37.9% rise in new patient visits subsequent to
private equity acquisition.4 Although a potential cause
for concern on rising healthcare costs, these statistics are not
necessarily bad. If PE-backed providers are improving access to
care, increasing clinical interaction, and addressing unmet demand,
these expenses will likely decrease the cost of emergent care in
the future. Additionally, technology investment may allow for
AI-powered care coordination that may also yield benefits and
reinforce the tenants of value-based reimbursement.
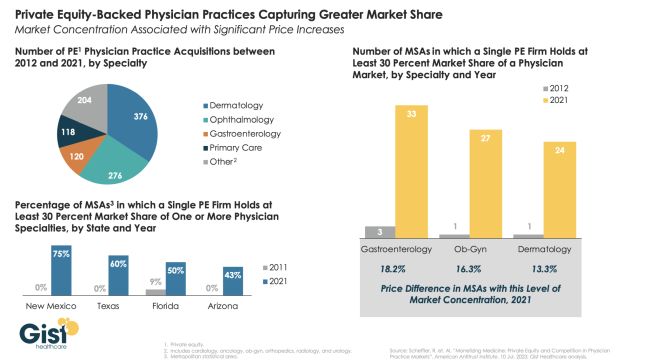
Image Source: Gist Healthcare, Private equity-backed
practices flexing market share muscle, September 2023[5]
A study conducted by Gist Healthcare5found
significant concentrations for PE-backed practices (defined as
greater than 30% market share) in over a quarter of the U.S. These
concentrations tend to be more pronounced in states with fewer
regulations and fast-growing senior populations.
Additionally, the study found higher healthcare prices in highly
concentrated markets with PE acquisitions. As an example, the study
showed an 18% price increase for gastroenterology in metropolitan
areas with high PE concentrations.5
How health systems can respond
Similarly, health systems can look not just at large practices
as acquisition targets but expand their sights to see if there are
multiple small practices that make sense to purchase and bundle
together.
2. Private equity firms focus on specialty clinics to create
vertical integration.
Certain specialties expect to see an increased demand for care
due to the demographics of an aging population, concurrent with a
provider shortage in those specialties. A prime example is urology,
which is currently an attractive investment target.6
Other sectors of interest such as dermatology, orthopedics,
gastroenterology, and allergy are preferred because they are
procedure-heavy and/or have investments in ambulatory surgery
centers (ASCs) that allow them to collect facility fees that are
often much higher than the reimbursement for a procedure in a
physician office setting. These high-margin procedures or
treatments can greatly increase profitability and help shift to a
more favorable payer mix.7
In the case of ophthalmology, not only are PE firms interested
in practices that own ASCs but also in vertically integrating
specialties such as optometry, ophthalmology, and retina
specialists. The combination of these specialties can provide
cross-referral opportunities and a comprehensive solution for
patients.2
How health systems can respond
Health systems can emulate the private equity playbook by
consolidating fragmented physician practice markets. A potential
avenue would be to establish hubs or centers of excellence for
certain specialties to attract target physicians with coordinated
care and improved patient access. Additionally, health systems can
target certain surgical specialties and increase
‘stickiness’ by prioritizing partnerships or joint ventures
with physicians on ASCs.
3. Private equity firms are gaining first-mover advantages in
value-based care
Private equity firms also favor primary care clinics and
“payviders” due to their central position in value-based
care. With many payers emphasizing value-based care and a continuum
of patient care, private equity companies can offer proficiency
with risk-based contracting and value-based care to bring
efficiencies to healthcare and increase access.6
Payers, funded by private equity, are making a long-term play in
value-based care and recognizing that patient health outcomes are a
critical component of their profitability. Active engagement with
patients through preventive medicine and a greater emphasis on
addressing the social determinants of health outside the
traditional purview of medicine can lead to higher
profits.8 Additionally, health plans recognize a
financial incentive to invest in retail, urgent care, and
after-hours centers to keep their members out of more expensive
emergency departments.9
For example, Oak Street Health reports a 50% reduction in
hospital admissions among its at-risk patients and a 42% reduction
in 30-day readmission rates. Half of Oak Street’s patients have
either a housing, food, or isolation risk factor.10
The key to being successful in the healthcare ‘new
world’ is to focus on best-in-class outcomes and lower costs.
Although reimbursement has not caught up, PE firms are
banking on the idea that having a developed and tested strategy in
the value-based world may pull government payers closer to the
value-based care model. They also know that it is
highly likely that the early adaptors in this space will tend to
reap the largest benefits. They expect government payers will start
with targets that are at or near their current cost and pare those
down as evidence and data prove cost reduction through care
management.
PE firms are fueling the transition to value-based care
with technology
Private equity investors are a natural partner to facilitate the
transition to value-based care due to their availability of capital
to drive investments in data and outcome management.6
The technology shift in healthcare and interoperability for
electronic medical records (EMR) systems has increased the usage of
data analytics to coordinate care across populations. Due to the
large capital investments needed for advanced EMR systems, data
analytics, and population management, physicians are realizing that
increasing size and scale is crucial for remaining competitive in
the modern healthcare environment.11
How health systems can respond
Healthcare organizations have several advantages in leading the
transition toward value-based healthcare. Healthcare organizations
are financing CMS waiver initiatives, through which they establish
partnerships with physicians to improve outcomes and reduce costs,
in anticipation of forthcoming reimbursement shifts. Alternatively,
healthcare organizations that qualify for incentive payments from
third-party payers can allocate a portion of the shared savings to
the physicians who played a role in achieving the improved
outcomes.
4. Private equity firms offer attractive buyouts and equity
models
PE firms can often offer large buyouts for physician practices,
many times at double-digit multiples of earnings. These large
buyouts are typically accompanied by reductions to future physician
compensation, reductions in overhead, and/or improved efficiencies
in administrative functions.3
Secondly, private equity generally can offer the upside of a
stock option. Typically, PE firms purchase a majority interest in a
practice but still allow the physicians some equity in the
practice. This gives the physicians some “skin in the
game” regarding future growth. Also, PE firms generally
anticipate a future sale in a three-to-five-year timeframe, and the
physician equity holders can benefit from the future sale of the
practice.2
How health systems can respond
While health systems are often constrained by regulations, there
are several avenues available to compete with the financial
incentives offered by private equity. First, health systems should
highlight that PE purchase and compensation strategies can create
dichotomies that may weaken a group as equity participants and
employed (generally younger) physicians who have a broadly
different benefit from the sale.
In addition, apart from the financial advantages that the
private equity model might provide, collaborating with healthcare
systems can yield various benefits for medical practitioners.
Generally, healthcare systems operate with extended strategic
planning horizons, affording them the ability to engage physicians
for more extended periods. This can prove highly advantageous for
physicians who prioritize stability or are dedicated to advancing
value-based healthcare models. Moreover, whereas most private
equity models concentrate on a specific medical specialty,
physicians aligned with a healthcare system often enjoy greater
integration with colleagues from a diverse array of specialties.
This interconnectedness can be inherently fulfilling and enhance
the coordination and administration of patient care.
“If you can’t beat them, join
them”
Ultimately, health systems may choose to partner with private
equity rather than directly compete. Coincidentally, this strategy
played out similarly between health systems and ASCs. Historically,
health systems were in fierce competition with ASCs. Health systems
argued that ASCs were selectively attracting the more profitable
surgical cases, while ASC operators maintained that ASCs offered
low prices, high quality, and patient convenience. While this
competition is still fierce in some markets, many health systems
are now partnering with physicians and ASC managers through joint
venture ASCs.
As reported in one recently published survey published in 2018,
41% of health system respondents “own or are affiliated with a
freestanding ASC.”13 Particularly interesting, of
those hospitals or health systems with current ASC ownership or
affiliations, 48% “anticipate making additional ASC
investments/affiliations in the coming years.”
Increasingly, there are newly emerging strategies such as health
systems taking part in a regional Management Service Organizations
(MSO), or in an ambulatory strategy with a third-party investor. In
this model, the health system participates in the underlying
capitalization table of the PE platform. Differing from an
independent contractor arrangement or traditional employment model,
the MSO structure can offer value to physicians. Health systems can
consider the advantages that joining with PE companies can offer to
enhance their physician alignment strategy.
Conclusion
Private equity investments in healthcare have accelerated the
shifting dynamics of the modern healthcare industry. Private equity
has pushed consolidation, vertical integration, and the transition
to value-based care. Moreover, their large capital resources have
attracted many physician practices and further fueled the
technological shift in healthcare.
Consumers’ expectations are evolving faster than
health systems can meet them. Driven in large part by
advances in other sectors, like banking, hospitality, logistics,
and other service industries, consumers expect to see the benefits
of technology in the healthcare setting, including basic
functionality — making appointments via an app, getting test
results rapidly and on one’s mobile device, and being able to
communicate with the care team through multiple modalities of
virtual communication.
Health systems need to play offense when confronted with these
new market forces. Because, in our experience, health systems that
effectively play offense are more successful. Understanding the
playbook of private equity investment, emulating it, and/or
partnering with it, is a good offense.
Footnotes
3. Potential Implications of Private Equity
Investments in Health Care Delivery – PMC (nih.gov)
4. Physician Practice Costs Grew 20% After Private
Equity Acquisition (revcycleintelligence.com)
5. Private equity-backed practices flexing market
share muscle – Gist Healthcare
8. Payers: A Shift from Insurance to Services | Bain
& Company
9. Market_Insights_MD_Ownership_Models.pdf
(aha.org)
10. Social-Impact-2021-Report.pdf
(oakstreethealth.com)
11. Hot physician specialties for private equity
investment (beckersspine.com)
The content of this article is intended to provide a general
guide to the subject matter. Specialist advice should be sought
about your specific circumstances.